The Centers for Medicare and Medicaid Services (CMS) has reissued transmittal instructions for Medicare Administrative Contractors (MACs) to perform a 5-claim probe and educate medical review on every skilled nursing facility (SNF) in their jurisdiction. The purpose of this widespread review, which will be implemented in waves over the next year beginning June 5, 2023, is to lower the SNF improper payment rate. Providers should be on the lookout starting in early June for medical records requests related to this program.
The key elements of this project include:
- All MACs that review SNF Medicare claims.
- MACs will select five (5) claims from each selected provider unless they are already under review or a very low volume provider.
- MACs will complete one (1) round of probe and educate for each selected provider instead of the potential three (3) rounds as instructed by the traditional targeted probe and educate (TPE) program.
- Education offered will be individualized based on the claim review errors identified in the probe.
This will be a pre-pay review unless a provider requests a post-pay review for hardship. If the MAC identifies an improper payment, it will adjust the individual claim payment, as appropriate, in addition to providing education – including the explanation for denial or payment adjustment. MACs may prioritize providers with errors in all five claims reviewed for the traditional and more extensive TPE program.
Background and Details
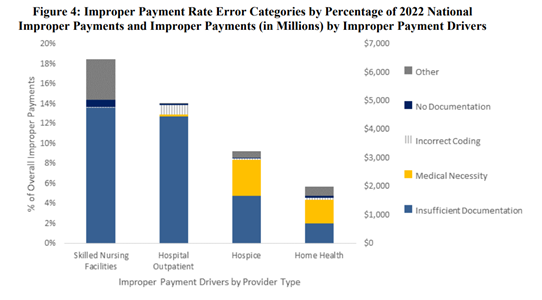
Per CMS, the Comprehensive Error Rate Testing (CERT) program for SNFs (skilled nursing facility) projected an improper payment rate of 15.1 percent in 2022 (see Figure 4 from the CERT report below), up from 7.79% in 2021. SNF service errors were determined to be the top driver of the overall Medicare Fee-for-Service improper payment rate. CMS states that part of the reason for the significant increase in the improper payment rate may be the change from the Resource Utilization Group (RUG) IV to the PDPM (patient driven payment model) for claims with dates of service on or after October 1, 2019. The primary root cause of SNF errors was found to be missing documentation (as depicted in Table 1 from the CERT report below).
CMS asserts that the 5-claim probe and educate review is an attempt to increase comprehension of correct billing practices under the PDPM by all SNF providers that bill Medicare. The 5-claim probe and educate medical review strategy allows for maximum outreach to all SNFs and offers provider-specific education, as necessary, to prevent future improper payments. If the MAC identifies an improper payment the MAC will adjust/deny the individual claim payment, as appropriate, and provide education.
Specific Details of the 5-Claim Probe and Educate Review
The specific instructions CMS provided to the MACs for the special review impacting providers include the following:
- How Samples are Selected and Review Process is Implemented
- Contractors shall select a sample of 5 claims for prepayment review (with occasional post-pay, if requested by the provider due to financial burden) from the universe of claims for all SNFs that submit claims for Medicare SNF services within the contractor's jurisdiction.
- The contractors shall implement the SNF 5-claim reviews on a rolling basis beginning with the top 20% of providers that show highest risk based on MAC data analysis.
- Contractors shall exclude providers/suppliers under review by other contractors.
- How Providers are Notified of Review Results and MAC Provider Education Responsibilities
- After an individual provider's 5 claim sample is completed, contractors shall send detailed results letters. NOTE: This requirement shall include sending result letters to providers with no error findings. CMS minimally expects detailed results letters to include individualized, claim-by-claim denial rationales (which may be based on the CMS provided denial dispositions), and it encourages contractors to include the written clinical details which must be discussed during the 1:1 telephonic education.
- For providers with an error rate of 20% or less (1/5 claims in error), MACs shall provide widespread education with the option for the provider to receive 1:1 education, if requested. NOTE: This offer letter shall clearly indicate a specific phone number and/or point of contact for providers to request education.
- For providers with error findings >20% in their sample, contractors shall offer 1:1 education in their results letter. NOTE: MACs shall reach out to the provider to schedule education if 2 or more claims in error.
- When the provider accepts 1:1 education the MACs shall provide education that includes claim specific information (i.e., clinical facts and corresponding denial reasons) and that allows the provider the opportunity to review the claim decisions, ask questions and receive meaningful feedback conducive to behavioral change and increased provider compliance.
- Contractors shall notify providers at the start of every teleconference that the discussion may be monitored by CMS as a third party for quality assurance purposes.
- Other Technical Guidance to the MACs
- The MAC shall no longer include in the provider notification letter language informing the provider that they can request additional time to respond to the ADR should they be experiencing burden.
- The MAC should accept documentation received after 45-calendar days for good cause. Good cause means situations such as natural disasters, interruptions in business practices, or other extenuating circumstances that the contractor deems good cause in accepting the documentation.
- The MAC shall close the round of review if 5 claims are not billed within 12 months.
- The MAC shall use their easily curable error processes should reviewers identify an easily curable error, and have a mechanism for reaching a provider/supplier point of contact that may be able to provide the compliant documentation.
- For dates of service during the PHE only, the MAC shall exclude claims containing the COVID-19 diagnosis, when possible.
- For claims with dates of service during the PHE, if the COVID-19 diagnosis does inadvertently fall into a sample, the MAC shall release the claim if identified during review.
- The MAC shall apply any applicable flexibilities and waivers when reviewing claims for dates of service after March 1, 2020, until the end of the Public Health Emergency. Note: These flexibilities and waivers can be found here.
- Instructions to MACs Regarding Providers with 5/5 Claims in Error
- The MAC shall prioritize for TPE review for providers who at the conclusion of the SNF 5 claim review project have 5/5 claims in error, if SNF is included in their existing Medical Review Strategy.